Mpox, previously known as monkeypox, is a viral disease caused by the poxvirus, a close relative of the variola virus that causes smallpox. As health concerns rise globally, understanding this virus has never been more critical. This guide aims to shed light on Mpox, offering a comprehensive overview of its origins, symptoms, transmission, treatment, and prevention strategies. By diving deep into this topic, you’ll be better equipped to understand and manage any potential risks associated with this emerging virus.
Understanding Mpox: A Close Look at the Poxvirus
The poxvirus is a large, complex virus with a distinct brick-shaped structure. It belongs to the Orthopoxvirus genus, which also includes the variola virus (smallpox) and the vaccinia virus (used in the smallpox vaccine). Mpox is a zoonotic virus, meaning it can be transmitted from animals to humans, but it can also spread from person to person under certain circumstances.
Mpox was first discovered in 1958 when outbreaks occurred in colonies of monkeys kept for research, hence the name “monkeypox.” However, its primary reservoirs are thought to be rodents and other small mammals. The first human case of Mpox was recorded in 1970 in the Democratic Republic of the Congo, and since then, it has been reported in various countries, primarily in Central and West Africa.
The Origins of Mpox: Tracing the Roots
Mpox’s history is deeply intertwined with that of smallpox, one of the deadliest diseases in human history. The eradication of smallpox in 1980 was a significant achievement, but it also left a void that Mpox began to fill in certain regions. With no smallpox virus to compete with, the poxvirus that causes Mpox started emerging more frequently.
The virus is endemic to several African countries, including the Democratic Republic of the Congo, Nigeria, and Cameroon. It thrives in tropical rainforests where humans and animals live in close proximity. As deforestation and urbanization encroach on these habitats, the likelihood of human exposure to the virus increases.
How Mpox Spreads: Modes of Transmission
Understanding how Mpox spreads is crucial for preventing its transmission. The virus can spread through:
- Animal-to-Human Transmission: This occurs when a person comes into direct contact with the blood, bodily fluids, or skin lesions of an infected animal. Consuming undercooked meat of infected animals can also lead to transmission.
- Human-to-Human Transmission: Although less common, Mpox can spread from one person to another through respiratory droplets during prolonged face-to-face contact. It can also spread through contact with contaminated materials, such as bedding or clothing.
- Indirect Transmission: Touching objects or surfaces that have been contaminated by the virus can lead to infection, although this is less common.
Identifying Symptoms: Recognizing Mpox Early

Early detection of Mpox is key to managing and treating the disease effectively. The symptoms of Mpox are similar to those of smallpox but generally less severe. The incubation period (the time from infection to the onset of symptoms) typically ranges from 7 to 14 days but can extend to 21 days.
The progression of symptoms usually follows this pattern:
- Initial Symptoms: The onset is marked by fever, headache, muscle aches, and exhaustion. Some patients may also experience chills and swollen lymph nodes, which is a key difference from smallpox.
- Rash Development: A few days after the fever begins, a rash develops, often starting on the face before spreading to other parts of the body. The rash evolves from macules (flat lesions) to papules (raised lesions), vesicles (fluid-filled lesions), and finally to pustules. These pustules eventually crust over and fall off.
- Recovery: The illness typically lasts 2 to 4 weeks. Most patients recover fully without treatment, but in some cases, especially among children and individuals with weakened immune systems, complications can occur.
Diagnosis and Testing: Confirming Mpox Infection
If Mpox is suspected, laboratory testing is essential to confirm the diagnosis. The most common diagnostic method is polymerase chain reaction (PCR) testing, which detects the virus’s genetic material. Samples are usually taken from the skin lesions, as they contain the highest concentration of the virus.
In areas where Mpox is endemic, healthcare providers may also consider serological tests, which detect antibodies against the virus in the blood. However, these tests are less commonly used because they cannot distinguish between an active infection and a past exposure to the virus.
Treatment Options: Managing Mpox Effectively
Currently, there is no specific treatment for Mpox. The management of the disease focuses on alleviating symptoms and preventing complications. This includes:
- Supportive Care: Patients are provided with fluids, pain relievers, and fever reducers to manage symptoms. In severe cases, hospitalization may be required.
- Antiviral Medications: While no antiviral drugs are specifically approved for Mpox, some medications used to treat smallpox, such as tecovirimat (ST-246), may be effective. These are typically reserved for severe cases or patients with weakened immune systems.
- Preventing Secondary Infections: Ensuring that the patient’s skin remains clean and dry can help prevent bacterial infections of the lesions.
Preventive Measures: How to Protect Yourself from Mpox
Prevention is the most effective strategy against Mpox. Since it is a zoonotic virus, reducing the risk of animal-to-human transmission is crucial. Here are some preventive measures:
- Avoid Contact with Wild Animals: Especially in regions where Mpox is endemic, avoid handling wild animals or consuming bushmeat.
- Practice Good Hygiene: Wash hands frequently with soap and water, especially after contact with animals or people who are sick.
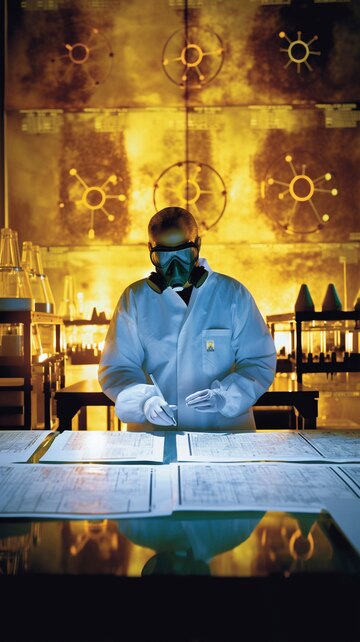
- Use Protective Gear: Healthcare workers and others who may come into contact with the virus should use personal protective equipment (PPE) such as gloves and masks.
- Isolate Infected Individuals: If someone is suspected of having Mpox, they should be isolated from healthy individuals to prevent the spread of the virus.
- Vaccination: The smallpox vaccine has been shown to be about 85% effective in preventing Mpox. In some cases, healthcare workers and others at high risk may be vaccinated as a preventive measure.
Global Response: How the World is Tackling Mpox
The global response to Mpox has been shaped by lessons learned from the smallpox eradication campaign. Various international organizations, including the World Health Organization (WHO), are actively monitoring the situation and providing guidance to countries on how to manage and prevent outbreaks.
Efforts include:
- Surveillance: Enhanced monitoring in regions where Mpox | Poxvirus Mpox is endemic helps detect and respond to outbreaks quickly.
- Public Health Campaigns: Educating the public about the risks of Mpox and how to prevent it is crucial in reducing transmission.
- Research and Development: Ongoing research is focused on developing more effective treatments and vaccines specifically for Mpox.
Mpox in the Modern World: The Impact of Globalization
Globalization has significantly impacted the spread of Mpox. Mpox | Poxvirus Increased travel and trade mean that viruses can cross borders more easily than ever before. Although Mpox is primarily confined to Central and West Africa, international travel has led to cases being reported in non-endemic countries, including the United States, the United Kingdom, and Israel.
This global spread highlights the importance of international cooperation in managing infectious diseases. Countries must work together to share information, resources, and strategies to prevent and contain outbreaks.
The Role of Vaccination: A Shield Against Mpox
Vaccination remains one of the most powerful tools in preventing the spread of Mpox. The smallpox vaccine, which led to the eradication of smallpox, has also been effective in preventing Mpox. However, since routine smallpox vaccination was stopped after the disease was declared eradicated, many people born after 1980 are not vaccinated and are therefore more susceptible to Mpox.
In response to the recent rise in cases, some countries have Mpox | Poxvirus considered reintroducing the smallpox vaccine for high-risk populations. Research is also ongoing to develop a more specific vaccine for Mpox that could provide even greater protection.
Mpox and Public Health: A Call to Action
Public health agencies worldwide recognize the threat posed by Mpox and are taking action to mitigate its impact. This includes strengthening healthcare systems in affected regions, improving diagnostic capabilities, and increasing access to vaccines and antiviral medications.
Community engagement is also essential. Educating the public about the risks of Mpox and how to prevent it can reduce fear and stigma associated with the disease. Empowering communities to take control of their health is a key component of any successful public health strategy.
Common Myths About Mpox: Separating Fact from Fiction
As with many emerging diseases, Mpox is surrounded by myths Mpox | Poxvirus and misinformation. Here are some common misconceptions:
- Myth: Mpox only affects monkeys.
Fact: While Mpox was first discovered in monkeys, it is primarily spread by rodents and other small mammals. - Myth: Mpox is always fatal.
Fact: Mpox is generally less severe than smallpox, and most people recover fully without treatment. - Myth: There is no way to prevent Mpox.
Fact: Vaccination, good hygiene, and avoiding contact with infected animals can significantly reduce the risk of infection.
Your Ultimate Guide To Discover Mpox | Poxvirus: Final Thoughts
Mpox is a disease that continues to challenge public health systems, especially in regions where it is endemic. Understanding the virus, how it spreads, and the best ways to prevent and treat it is essential for managing the risk it poses. As the world becomes more interconnected, the importance of global cooperation in combating diseases like Mpox cannot be overstated.
By staying informed and taking proactive steps, individuals and Mpox | Poxvirus communities can protect themselves from this emerging threat. Remember, knowledge is your best defense against Mpox and other infectious diseases.
FAQs
What is Mpox, and how is it related to the poxvirus?
Mpox is a viral disease caused by the poxvirus, which is closely related to the variola virus that causes smallpox. It was initially discovered in monkeys but is primarily spread by rodents.
How does Mpox spread between humans?
Mpox can spread from person to person through respiratory droplets during close contact, direct contact with bodily fluids or lesions, and contact with contaminated materials.
What are the symptoms of Mpox?
Symptoms include fever, headache, muscle aches, swollen lymph nodes, and a characteristic rash that progresses from macules to pustules before crusting over.
Is there a treatment for Mpox?
There is no specific treatment for Mpox. Management focuses on Mpox | Poxvirus supportive care and, in some cases, the use of antiviral medications like tecovirimat.
Can Mpox be prevented through vaccination?
Yes, the smallpox vaccine is about 85% effective in preventing Mpox. In some cases, it may be recommended for high-risk individuals.
Where is Mpox most commonly found?
Mpox is most commonly found in Central and West Africa, particularly in the Democratic Republic of the Congo, Nigeria, and Cameroon.